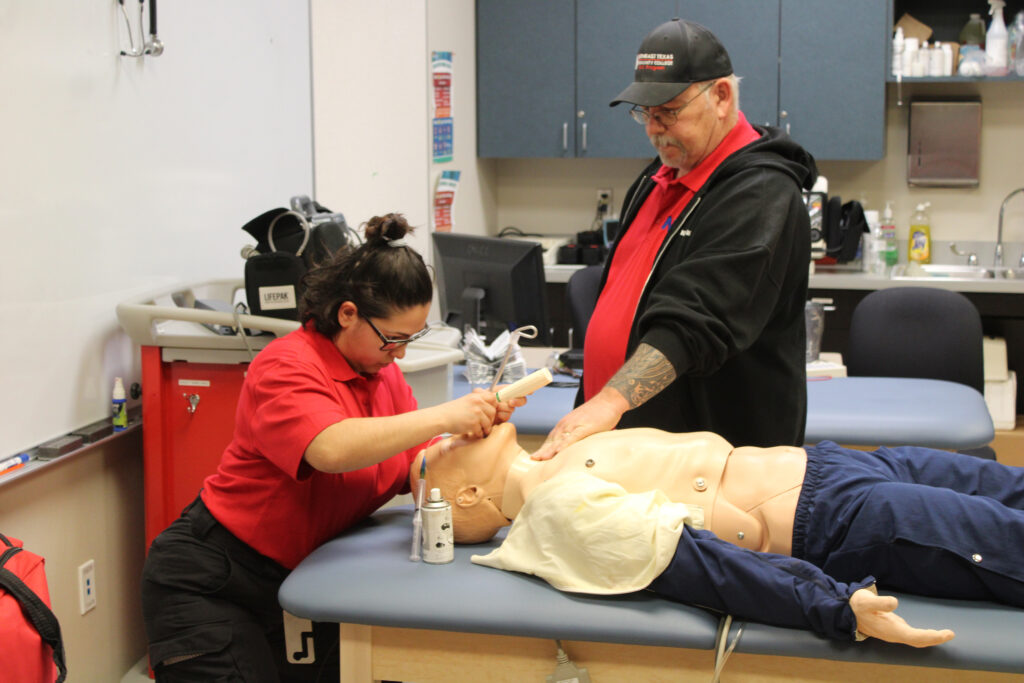
EMS student Graciela Salinas practices intubating a sim lab mannequin while Instructor Ray Ford watches. (Staff Photo | Joelle Weatherford)
By Skylar Hodson
Staff Writer
The job of EMS First Responders can be demanding, not just physically, but emotionally and mentally as well.
They are often the first people on the scene of an accident, witnessing gruesome sights, sounds and smells that most people would never dream of seeing.
These experiences often put strain on their mental health, sometimes resulting in post-traumatic stress disorder.
EMS workers struggling with PTSD may find it difficult to improve their mental health for several reasons. One of these reasons could be that they lack knowledge of available resources.
Other reasons could include thinking that asking for help is a sign of weakness or believing that only military members can suffer from PTSD.
At NTCC, EMS professors Gary Short and Russell VanBibber, along with professor of psychology, Jennifer Sutton, are doing their part to help raise awareness of these issues by teaching their students about them.
As a professor of psychology, Sutton understands the importance of mental health awareness.
“In recent years, we have seen a number of celebrities talk openly about their own mental health issues and treatment,” Sutton said. “That seems to have led us to a place in which non-celebrities can also talk more openly about mental health issues.”
Increasing awareness about mental health issues and treatment can help anyone struggling with PTSD.
The American Psychological Association says PTSD can develop after “experiencing or witnessing traumatic events” that pose a “significant physical, emotional or psychological threat” to an individual or their loved ones.
Symptoms of PTSD include having “intrusive or recurrent memories of the trauma” such as nightmares, “trouble sleeping or concentrating,” and “feeling sad, angry or numb.”
The APA also says PTSD symptoms lasting over a year “probably won’t resolve on their own,” and “it is never too late to be treated for PTSD.”
Sutton recalled a time when she had difficulty finding affordable resources for a non-military student struggling with PTSD.
While she was not helping an EMS worker, she acknowledged trouble finding available resources could interfere with first responders receiving assistance for PTSD.
Failure to receive help may cause mental health issues to worsen. According to the APA, untreated PTSD can contribute to depression, chronic pain and substance abuse.
According to a 2021 eurekalert.org peer-reviewed publication, EMS workers are “three times more likely to experience mental health issues,” such as depression and PTSD, compared to members of the general population.
As EMS professors with many combined years of work in the field, both Short and VanBibber are intimately familiar with the effects the job can have on the mental health of an EMT or Paramedic.

NTCC EMS student Scott Stansell, left, works on improving his time after getting third place in the class’s intubation timed competition. Part of the students’ training is also learning how to cope with the mental stress that comes as a first responder. (Staff Photo | Skylar Hodson)
EMS workers face potentially traumatic incidents on a daily basis. Short said the way he teaches students to handle these experiences is not the same as he was once taught.
“Back then they didn’t do a good job of prepping you for dealing with everything that you’d see,” Short said. “It didn’t give me good tools to use to be able to keep me from suffering from the ill effects of PTSD. It let me go down the depression road that was kind of long and dark.”
Short now tries to properly prepare students to face these stressors. Short shares his own personal experiences with PTSD and depression and encourages his students to seek help. He reminds them that reaching out to others is not a sign of weakness.
“I try to make it as small an impact on them as I possibly can and prepare them for things that they may see or hear.”
One way VanBibber prepares his students is by giving them advice to help them manage their emotions during stressful calls.
“If you go to a scene and it looks really bad, put your fingers on your neck,” VanBibber said. “If you see a pulse, you’re good, work on the people who aren’t. You’re going to see some things that are going to bother you, but they have to bother you later.”
Throughout the years, Short and VanBibber have prepared many students to handle the difficulties accompanying calls. Daniel Moss, NTCC Paramedic student and Navy veteran, discussed how this training helped him stay calm and collected on the job.
“The first thing you’ve got to really do, as a First Responder or anything, is you have to keep telling yourself that it’s their emergency, it’s not yours,” Moss said. “So it helps you when you’re out in the field to get in the proper mindset of ‘I need to do what I’ve been trained to do, I need to do what I’ve learned, that way I can help them.’
“If you’re out there stressed out to begin with on a call, you’re freaking out on it, you’re not going to be any good to the patient or yourself.”
Moss said the training changed his mindset on talking about mental health. This later proved to be a valuable change, as it enabled him to reach out for help.
“When I first got into the military it was still the old-school mindset of ‘get over it and just get your job done,’” Moss said. “Nobody ever talked about it because, to them and to that generation, it was a sign of weakness if you talked about ‘this messed me up.’ But after getting into EMS I actually had an amazing partner, and she was amazing as far as talking about it.”
When it comes to resources available for EMS workers, there is a wide variety they can turn to in their time of need. Moss talked about the importance of having outlets such as talking to people you feel comfortable with.
While Moss was an active EMT, he considered his partner one of his best resources, since talking to her allowed both of them to process what they had been through.
“As soon as the call was over, she and I talked about the call and what was going on. We were able to break it down between the two of us as in ‘Yes, it was a call that was very traumatic to see,’ or ‘It was a call that was really emotional,’ but we were able to talk about it between the two of us. It was great because I had a partner that understood how it would affect you later on, and that was the key element to that, was having a partner who understands that.”
Professor VanBibber also recommends talking to someone in order to process how you feel.
“There are issues with seeing what you see and you have to be able to let it go by talking.”
However, before talking to family members about EMS experiences, he recommends talking to someone who might better understand, such as a boss, coworker, or a professional.
He said that Crisis Management Teams are a great resource for EMS workers to use.

Local EMS paramedics perform a medical airlift demonstration for children during the NTCC Kid’s Camp held last summer. This activity highlights just some of the duties regularly performed by EMS workers. (Staff Photo | Joelle Weatherford)
Anyone can struggle with PTSD, even students who are not going into the EMS field. With that in mind, Professor Sutton compiled a list of resources for those in need of help.
“Websites such as talkspace.com, talkiatry.com, betterhelp.com, and ptsd.va.gov (for military) offer a variety of mental health services,” Sutton said.
Resources are valuable tools for anyone in need of help, but an individual must first be willing to reach out in order to receive their assistance. All three professors agree that asking for help does not make the individual weaker or lesser than anyone else.
Sutton said there are many different kinds of people who can help.
“There are trained professionals who have the skills and tools to equip you to begin healing,” Sutton said. “There are those who have faced similar struggles and can offer encouragement. And there are still others that will help in whatever way they can physically, emotionally, financially.”
Recalling past acquaintances who lost their battle with PTSD, Moss emphasized just how important it was to ask for help, warning about the risks of dealing with your mental health alone.
“I’ve lost 23 people from Afghanistan alone to those kinds of issues,” Moss said. “They were in that mindset of ‘I can deal with it on my own, I don’t need anybody else’s help and I don’t need to talk about it.’”
Short said there are many ways to relieve stress caused by mental health issues. And offered a stark reminder that suicide is never the solution.
“Others around you need you there, don’t think that a permanent solution to a temporary problem is the way to go,” Short said. “Always reach out, there’s somebody to reach out to.”
If you or anyone you know are struggling with suicidal ideation and want to get help, please call the National Suicide Prevention Lifeline at 1-800-273-8255.